What to Know About Intraoperative CT Bronchoscopy
Lung cancer is one of the most common types of cancers and it is the deadliest. Diagnosis and treatment of lung cancers have historically been challenging, but innovations in medical technologies have opened the door to new diagnostic procedures.
Intraoperative CT bronchoscopy technology offers significant benefits for patients and physicians alike.
Contact us today to learn more about Body Vision’s intraoperative CT imaging.
What is Intraoperative CT?
Computed tomography (CT) is a medical imaging technology that takes multiple 2D x-rays and then uses a computer imaging algorithm to create a detailed 3D scan of the human body. A CT scan can depict skeletal structures and organs, as well as blood vessels and glands.
Intraoperative CT leverages the power of computed tomography in the operating room, enabling clinicians to make informed operating decisions based on images and scans obtained during the procedure. Intraoperative CT imaging scans are critical in procedures involving the lungs, brain, and spine, among others.
Benefits of Intraoperative CT
Intraoperative CT offers a slate of benefits for medical professionals. First, intraoperative CT images give clinicians the ability to verify the success of a procedure immediately while patients are still in the procedure room.
The ability to verify the success of a procedure with intraoperative imaging can help to reduce the overall number of procedures that patients must undergo. Additionally, complications of moving patients out of the procedure room in order to conduct a scan are also reduced. Intraoperative CT technology allows CT scans to be brought directly to the patient rather than bringing the patient to the CT scans.
With intraoperative CT, clinicians can also easily monitor the amount of tissue removed during an operation or in the case of minimally-invasive procedures like bronchoscopy, visualize the precise area of interest.
What is Bronchoscopy?
Bronchoscopy is a procedure that allows doctors to view the airways of the lungs using medical instruments. The throat, larynx, trachea, and lower airways are typically examined using a bronchoscope. Bronchoscopy may be performed to diagnose lung cancers or treat lung problems.

Traditionally, there are two main types of bronchoscopes used to perform bronchoscopy, rigid and flexible.
Rigid bronchoscopes are used to view the largest airways and can be used to perform procedures such as:
- Removal of foreign objects
- Removal of lesions
- Implanting stents
Flexible bronchoscopes are used more often than their rigid counterparts, are more appropriate for smaller airways, and can perform procedures such as:
- Biopsies
- Suction
- Placing breathing tubes
Intraoperative CT Bronchoscopy: Most Common Practices
Typically, suspicious pulmonary lesions are either detected on low-dose CT screens or incidentally during chest x-rays. Once a suspicious lesion is identified, a biopsy of the tissue from within that lesion is taken to definitively diagnose whether or not cancer is present.
This biopsy is most commonly conducted via a transthoracic needle aspiration (TTNA) performed by an interventional radiologist or via diagnostic bronchoscopy performed by an interventional bronchoscopist or thoracic surgeon. If these two minimally invasive techniques prove unsuccessful in obtaining a definitive diagnosis and there is a high enough suspicion of lung cancer, a confirmatory diagnosis can also be obtained after the suspicious area is surgically resected by a thoracic surgeon.
As with many procedures, the more invasive the technique, the higher the likelihood of complications and the longer the recovery time.
In TTNA, an interventional radiologist, under CT-guidance, penetrates the chest wall with a needle to take a tissue sample of the suspicious lesion. Because of the intraoperative CT guidance which enables the radiologist to visually confirm that the biopsy needle is collecting tissue samples from within the lesion, this method has a high diagnostic success of greater than 90%.1 However, this comes with the risk of a pneumothorax or collapsed lung in nearly one in four patients that undergo the procedure1 and a corresponding hospital stay.
Alternatively, an interventional pulmonologist or thoracic surgeon can perform a minimally-invasive procedure called diagnostic bronchoscopy to obtain a biopsy. In this procedure, the clinician snakes a bronchoscope through the patient’s mouth and down the trachea into the lungs where a biopsy of the lesion can be taken.
While this method is minimally-invasive and comes with fewer potential complications, historically this approach has lacked real-time, intraoperative imaging and thus the diagnostic success rate is approximately 70%2. Unlike in TTNA, the clinicians performing bronchoscopy do not typically have access to intraoperative imaging and so cannot see exactly where the lesion is during the procedure nor can they confirm that they are acquiring tissue samples from within the lesion in real-time.
Intraoperative CT imaging enables bronchoscopists to achieve diagnostic outcomes similar to that achieved by interventional radiologists in TTNA using a far less invasive approach.
Intraoperative CT-guided bronchoscopy is becoming more widely adopted and there are several real-time, intraoperative imaging technologies available to bronchoscopists today.
The most common, though by no means widely adopted, is cone-beam CT (CBCT). CBCT is a computational tomographic X-ray imaging modality that allows for accurate, 3D imaging of tissue at a submillimeter resolution.
While more commonly used in orthopedics, spine surgery, and other disciplines for the imaging of bone and other dense anatomical structures, CBCT has seen some limited adoption in bronchoscopy as a means of providing real-time intraoperative imaging of both the lesion and tools during a bronchoscopic procedure, thus affording bronchoscopists similar CT guidance as their interventional radiology counterparts.
However, the cost of a CBCT system, the need for a dedicated hybrid operating room to house it, a comparatively high dose of radiation exposure for both clinical staff and patient for every CBCT scan performed, and competition for access, of which pulmonologists who perform bronchoscopy are typically lower in priority than other hospital lines of service, all hinder broader adoption by bronchoscopists.
The advent of 3D-capable C-arms, often referred to as “mobile cone-beam,” has endeavored to make CBCT more accessible to bronchoscopists. However, the technology remains newer and some of the issues with fixed CBCT systems such as high cost and comparatively high radiation exposure, still remain a concern. Moreover, these new 3D C-arms, while able to render 3D tomographic images, tend to also be of lower resolution than fixed CT systems and so cannot image soft-tissues and particularly smaller, less dense lung lesions, with the same fidelity as full-sized, fixed CBCT systems let alone full-fledged CT scanners.
The most recent addition to the real-time, intraoperative CT imaging armamentarium is Body Vision Medical’s LungVision™ system, which uses artificial intelligence (AI) to transform X-ray images from any C-arm into real-time, intraoperative CT scans which can be presented in different views that enable bronchoscopists to see both the lesion and their bronchoscopic tools in real-time during the procedure.
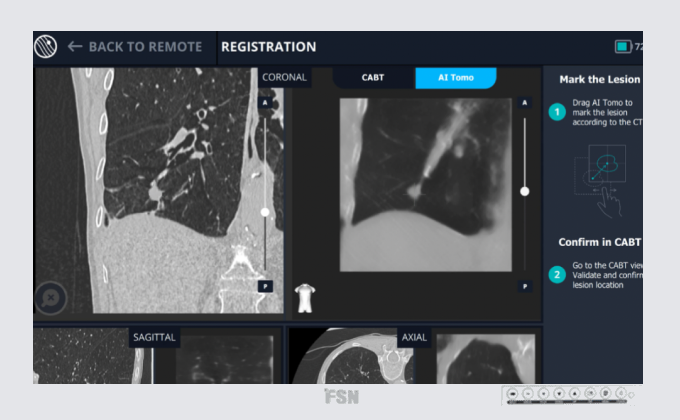
The first of these views is a multiplanar 3D view where the clinician can see the intraoperative CT scan in three planes, not unlike what they typically see in a CBCT or traditional CT scan. The latest iteration of this technology dubbed AI Tomography takes this one step further with an additional layer of processing that significantly enhances image quality and enables representation of the 3D image in the traditional axial, coronal, and planes familiar to clinicians.
The second way of presenting the 3D imagery is called 3D View and provides the clinician a 3D reconstruction that they can interactively manipulate to better understand the lesion-bronchoscope tool relationship needed to confirm tool-in-lesion prior to biopsy, or in cases where they do not have tool-in-lesion, how to go about repositioning the bronchoscope so that can achieve visual confirmation that they are biopsying from within the lesion.
Lastly, Body Vision’s augmented fluoroscopy provides a real-time, fluoroscopic X-ray view of the area of interest with overlays showing the actual lesion and lesion location. This provides clinicians a view of the lesion and their bronchoscopic tools in real-time.
Body Vision’s LungVisionTM system also provides navigational capabilities, enabling it to serve as an all-in-one diagnostic bronchoscopy solution that supplants electromagnetic navigation bronchoscopy (ENB) platforms or as a dedicated imaging platform that enhances robotic bronchoscopy platforms by providing real-time, intraoperative CT imaging that they lack.
Compared to other CT imaging methods like CBCT, Body Vision’s approach helps drive superior clinical outcomes by providing intraoperative imaging at significantly reduced cost with less radiation and greater accessibility. With multiplanar 3D view, interactive 3D View, real-time augmented fluoroscopy, and streamlined navigation, Body Vision’s intraoperative CT imaging maximizes the likelihood of achieving a definitive diagnosis, resulting in better outcomes for patients and healthcare facilities alike.
Body Vision's AI Tomography Imaging showing tool-in-lesion confirmation.
Contact us to learn more about Body Vision.
Intraoperative CT-Guided Bronchoscopy Procedure
Using Body Vision’s advanced real-time imaging technology, physicians can confidently access pulmonary lesions and take evidence-based samples, maximizing the likelihood of an early diagnosis for lung cancer patients and improving odds for survival.
Body Vision’s intraoperative CT bronchoscopy procedure involves five primary steps:
In pre-procedure planning, any suspected lesions are marked using CT scans and a pathway is planned to each lesion. This can be done at virtually any time of the physician’s choosing, before or after the patient is present in the operating room and takes minimal time.
The preoperative imaging is uploaded, lesions are identified, and lesion boundaries are marked. Powerful artificial intelligence technology is able to derive the airway branches from the preoperative CT scan and generates potential pathways to access the lesions. Physicians then choose which pathway is best.
A virtual bronchoscopy representation of the chosen pathway is shown to aid the bronchoscopist and staff to learn the particular aspects of the impending procedure and plan for any necessary challenges prior to starting the navigation.
The bronchoscopist then navigates out to the lesion with the bronchoscope using either the Body Vision system as the navigation system or their navigation platform of choice. Once at or near the lesion, a C-arm spin is performed so that the Body Vision system can provide an intraoperative CT scan to determine the exact lesion-bronchoscope relationship and to provide the visual information needed to navigate the “last mile” to the lesion. A biopsy tool can then be introduced down the working channel of the bronchoscope and, if further confirmation is needed, another C-arm spin can be performed to visually confirm tool-in-lesion prior to biopsy.
Once the distal tip of the biopsy tool has been confirmed inside the lesion, biopsy samples can be collected from within the lesion. Body Vision’s intraoperative CT imaging eliminates the need for taking biopsy samples from more locations than necessary. Physicians can confidently take samples directly from the lesion.
Intraoperative CT Bronchoscopy Potential Drawbacks and Considerations
Intraoperative CT bronchoscopy helps to ensure a streamlined procedure in the operating room with an incredibly high degree of diagnostic accuracy. Many doctors turn to this technology because of its cost-effectiveness and reliable performance. However, intraoperative CT bronchoscopy also comes with potential risks.
While a CT-guided bronchoscopy using an intraoperative CT scanner is less invasive than other biopsy techniques used in the operating room, complications can still arise.
A small number of patients may experience an air leak caused by biopsy instruments penetrating lung tissue. The damage is usually negligible and the hole typically heals of its own accord without the need for additional procedures.
In rare cases, a tube may need to be inserted through the chest wall to siphon air from the chest cavity. This procedure introduces the potential risk of infection since it involves a needle penetrating the skin. There is also a small risk of bleeding, as in many invasive procedures. Excess bleeding may require a blood transfusion.
Risks will vary depending on the overall health of the patient and their own unique risk factors. Patients with high levels of carbon dioxide in their blood or a history of breathing difficulty may need to be placed on a breathing machine prior to bronchoscopy.
Following a bronchoscopic procedure, patients will need to spend time in recovery. An intraoperative CT scan generally limits or even eliminates the need for additional x-rays because surgeons can verify the success of a procedure immediately following the operation. However, patients who have undergone other types of bronchoscopy may need additional medical imaging taken after the procedure.
Patients will likely experience mild discomfort in their throat and chest and cannot safely eat or drink until their gag reflex has returned. Strenuous physical activity after a bronchoscopy is discouraged but most patients will be able to return to normal activities and diet after a few days.
Intraoperative CT-guided bronchoscopy has provided success in many procedures and Body Vision’s technology has made a tremendous difference in the accuracy, cost-effectiveness, and accessibility of intraoperative CT, as demonstrated in an array of real-world case studies.
Biopsy and Diagnosis of 9mm Nodule in Right Middle Lobe
- A 67-year-old non-smoker was experiencing unexplained weight loss and underwent a CT scan
- Dr. Amir Abramovich, Director of Interventional Pulmonology at Carmel Medical Center, used Body Vision's real-time CABT technology to accurately locate the lesion and take a biopsy sample.3
Biopsy and Diagnosis of 25mm Right Upper Lobe Lesion
- An 88-year-old non-smoker with a remote history of breast cancer had undergone two previous attempts to biopsy a solitary pulmonary nodule in the right upper lobe but both attempts had proven nondiagnostic
- Dr. D. Kyle Hogarth at the University of Chicago Medical Center used Body Vision technology to see the lesion in real-time and successfully obtain biopsy samples.4
Biopsy and Diagnosis of a 12mm Lesion in the Right Upper Lobe
- A suspicious nodule was found in the right upper lobe of a 69 year-old current smoker with COPD during a routine CT screening
- Dr. Joseph D. Whitlwark, MD, used Body Vision technology in conjunction with Auris Monarch robotic bronchoscopy to navigate the target and retrieve tissue samples.5
The Body Vision Advantage
Body Vision Medical understands the threat that lung cancer poses to public health and has established its mission to save lives through the democratization of innovative medical technologies. Body Vision’s LungVisionTM imaging system is uniquely positioned to help healthcare institutions deliver on the quadruple aims of enabling existing medical staff to deliver superior clinical outcomes and patient experience at a lower cost.
Body Vision’s approach with LungVisionTM is to ensure that it works with existing imaging and bronchoscopy equipment a healthcare institution has so that we empower them to better serve a growing population of lung patients without ballooning overall operating costs. This allows institutions to cost-effectively drive superior clinical outcomes by providing intraoperative imaging at significantly reduced cost, reduced radiation, and much greater accessibility compared to CBCT.
For institutions who have already invested in robotic bronchoscopy, LungVisionTM maximizes the capabilities of the robot by enabling visualization of actual lesion and lesion location during the procedure to eliminate CT-to-body divergence and provide visual confirmation of tool-in-lesion prior to biopsy to fully leverage the stability and articulation benefits of robotics during navigation, biopsy and, in the future, therapy.
For institutions that are currently utilizing electromagnetics for navigation or currently lack any sort of navigation technology, LungVisionTM is an opportunity to acquire a next-generation platform that provides both image-guided navigation and real-time, intraoperative CT imaging in a single platform.
Body Vision’s AI-driven, intraoperative imaging platform can have a profound impact on the clinical and financial opportunities for healthcare institutions.
The immediate benefit of Body Vision's intraoperative CT imaging is maximizing the likelihood of obtaining a definitive diagnosis for lung patients at a higher rate. This higher diagnosis success rate results in greater patient retention with the system, driving high downstream revenue for thoracic surgery, radiation oncology, medical oncology and other lines of service. The acquisition of cutting-edge technology like intraoperative CT imaging also elevates the visibility of the lung program and can serve as a point of differentiation for an institution, driving growth in market share.
The benefit of a higher diagnostic rate for the patient is equally clear. It enables them to get the diagnosis they’re looking for with a minimally invasive bronchoscopic procedure that both reduces probability of complications, and thus, a potentially unplanned hospital admission as well as, if diagnosed the first time, shortens the patient journey by eliminating the need for additional diagnostic procedures.
The cost-effectiveness of the Body Vision technology also makes it more probable that the technology is economically viable for regional and community hospitals to acquire, increasing the likelihood that patients have local access to this technology versus needing to travel potentially great distances to major academic institutions in order to access the latest in technology.
From a medical provider standpoint, the introduction of intraoperative imaging greatly reduces uncertainty and complexity of the diagnostic bronchoscopy procedure, reducing overall procedure time and opening up the ability to treat more patients. Moreover, a higher performing pulmonology program potentially enables conversion of TTNA and surgical resection cases into bronchoscopy cases for patient diagnosis, which not only improves the patient experience with a less invasive procedure with fewer potential complications, but also frees up interventional radiology and thoracic surgery resources, respectively for additional procedures.
With over 2,500 patients who have already benefited from it’s AI-driven, intraoperative imaging technology, Body Vision is committed to partnering with institutions, physicians, and staff worldwide to improve lung cancer diagnosis so that lung cancer patients globally can have options and hope for longer, healthier lives.
- DiBardino DM, Yarmus LB, Semaan RW. Transthoracic needle biopsy of the lung. J Thorac Dis. 2015 Dec;7(Suppl 4):S304-16.
- Mehta AC, Hood KL, Schwarz Y, Solomon SB. The Evolutional History of Electromagnetic Navigation Bronchoscopy: State of the Art. Chest. 2018 Oct;154(4):935-947.
- Abramovich, A. (18 C.E., January). Biopsy and Diagnosis of 9mm Nodule in Right Middle Lobe. BodyVision. https://bodyvisionmedical.com/articles/abramovich-use-case-1
- Hogarth, K. (2022, March 21). Biopsy and Diagnosis of 25mm Right Upper Lobe Lesion. BodyVision. https://bodyvisionmedical.com/articles/biopsy-and-diagnosis-of-25mm-right-upper-lobe-lesion
- Whitlark, J. (2022, September 19). Biopsy and Diagnosis of a 12mm Lesion in the Right Upper Lobe. BodyVision. https://bodyvisionmedical.com/articles/crozer-health-whitlark-use-case
FAQs
- What is considered intraoperative?
- The intraoperative period involves the monitoring, anesthetization, preparation, and operation of the patient in the procedure room. “Intraoperative'' refers to any medical processes or activities performed during a procedure.
- What is CT in surgery?
- Computed tomography (CT) is a type of medical scanning technology that generates images using a combination of x-ray images taken from various angles. CT scans are used to provide highly-detailed images of bones, blood vessels, and soft tissues so surgeons can appropriately plan as well as execute surgical procedures.
- Why are CT scans ordered?
- Computed tomography (CT) scans may be ordered to assist doctors in properly diagnosing their patients. CT scans are used for a variety of medical purposes including pulmonology.