Image-Guided Bronchoscopy for Peripheral Lung Lesions
As lung cancer continues to threaten the health of millions globally, breakthrough medical technologies will play an increasingly vital role in diagnosis and treatment.
Biopsy samples from a pulmonary lesion are often difficult to collect through the use of conventional bronchoscopic techniques. By leveraging the power of image-guided bronchoscopy, physicians can more accurately place biopsy tools within the lesion prior to sampling and maximize diagnostic yield.
Are you interested in leveraging image-guided bronchoscopy technology to maximize your diagnostic yield? Contact us today.
Introduction
Pulmonary nodules can be difficult to biopsy using traditional bronchoscopy methods. There are several image-guided bronchoscopy techniques used today to support the successful sampling of pulmonary nodules. These techniques vary in their diagnostic yield, associated risks, and the clinical expertise required to perform them.
Definitions and Etiology
Generally speaking, image-guided bronchoscopy is a method of guiding bronchoscopic instruments to lung lesions through the use of an advanced imaging technology.
A pulmonary lesion is any abnormality in the lungs and is typically caught incidentally during a chest X-ray, or increasingly, in low-dose CT scans as lung cancer screening programs become more prevalent. While lung nodules may be an indicator of lung cancer, benign nodules are common. Lung nodules can vary in shape, size and type, and physicians follow specific guidelines in determining whether more testing, such as a PET/CT (positron emission tomography) scan or a lung biopsy, is warranted in order to arrive at a definitive determination of malignancy. Peripheral lung lesions, due to their location, are difficult to access for biopsy using conventional bronchoscopy methods.
Goals of Image-Guided Bronchoscopy
Image-guided bronchoscopy helps physicians more accurately navigate the bronchoscope to and collect biopsy samples from the pulmonary lesion by providing intraoperative imaging during the procedure so that the bronchoscopist can readily see the lesion and their tools throughout the procedure. Because such real-time, intraoperative imaging technology had not previously been widely available, diagnostic bronchoscopy, while safer and with fewer complications due to its minimal-invasiveness, has historically produced a lower diagnostic yield compared to more invasive diagnostic techniques such as transthoracic needle aspiration (TTNA) or surgical lung resection. Through the use of advanced imaging technologies, physicians can potentially make significant improvements in their ability to successfully diagnose lung patients via bronchoscopy.
Marking of the pulmonary lesion with fiducial markers or dyes so that it can be accurately targeted in subsequent radiosurgery or surgical resection is also often done during diagnostic bronchoscopy. Intraoperative CT imaging also aids precise placement of these marking aids.
The Bronchoscopy Procedure

In its simplest terms, bronchoscopy allows doctors to view the systems of the lungs including the throat, larynx, trachea, bronchi, and bronchioles using minimally-invasively with a bronchoscope. In some cases, image-guided bronchoscopy may also be used to provide guidance to central lymph nodes.
Bronchoscopies can be separated into two main categories based on the type of bronchoscopes used.
Rigid bronchoscopes are used to view the largest airways and aren’t appropriate for use in the more constrained lower airways due to their firm, rigid nature.
Though a rigid bronchoscope limits the range of possible diagnostic and therapeutic techniques performed, rigid bronchoscopes can be useful in
- Removing foreign objects from the lungs
- Controlling bleeding
- Suction of secretions
Rigid bronchoscopes are appropriate for certain procedures such as:
- Removal of foreign objects
- Removal of lesions
- Implanting stents
Flexible bronchoscopes are used more often than their rigid counterparts. This is because flexible bronchoscopes have greater articulation and can be maneuvered into varying airway depths of the lungs for more comprehensive diagnoses.
Flexible fiberoptic bronchoscopes also feature a hollow working channel through which specific procedures can be performed, including:
- Collecting tissue samples (biopsy)
- Delivering oxygen
- Vacuum suction
- Administering medications
Flexible bronchoscopes are used in procedures such as:
- Biopsies
- Suction
- Placing breathing tubes
Virtual Bronchoscopy
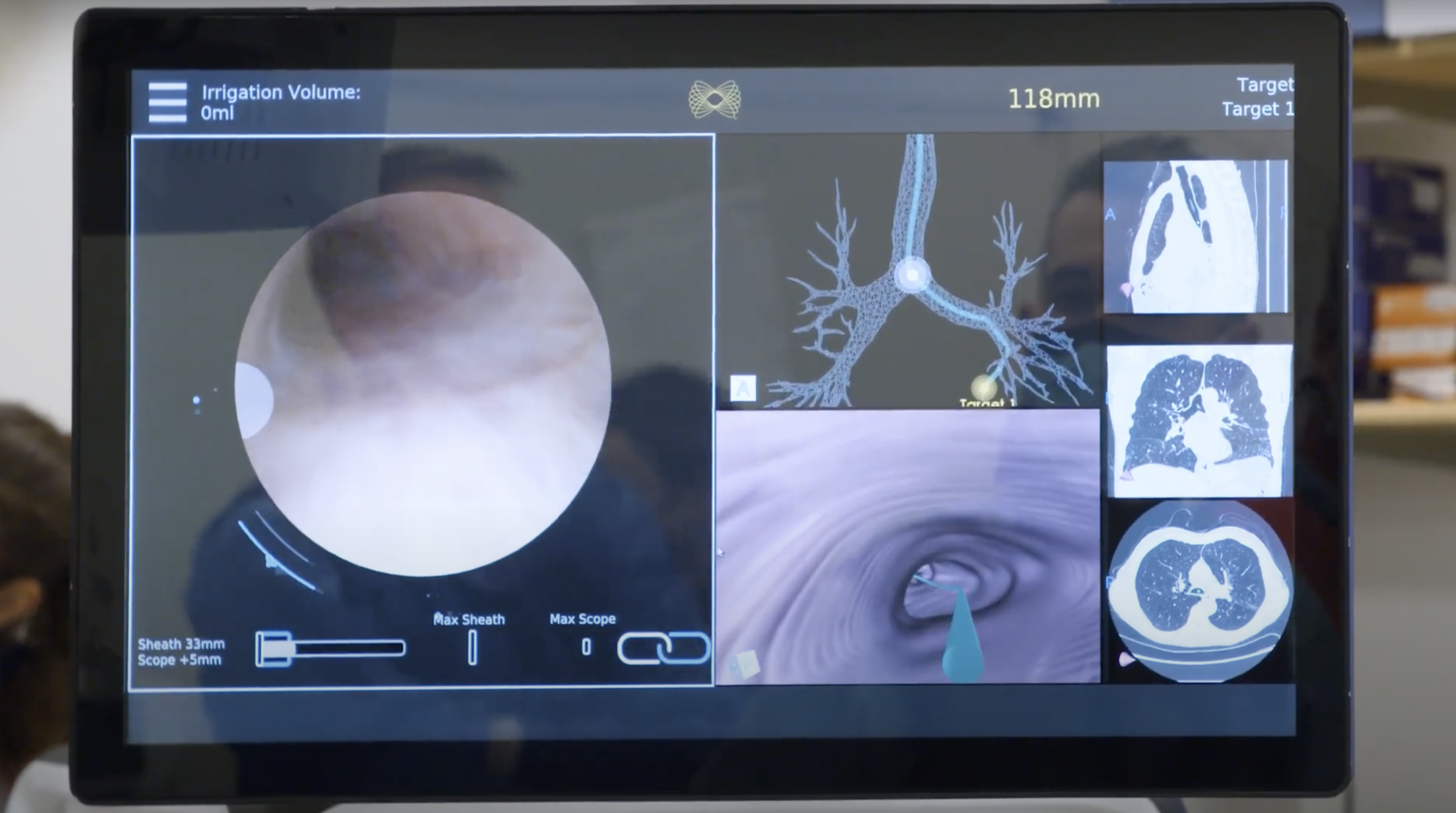
Virtual bronchoscopy uses non-contrast enhanced computed tomography (CT) images obtained preoperatively to create a virtual, three-dimensional representation of the airway tree. The imaging generated is comparable to that rendered from an invasive bronchoscopy procedure.
This enables the bronchoscopist to visualize the pathway to the target prior to the procedure and, during the procedure, provides the physician a 3D map to the target.
However, because the target is defined from the preoperative CT instead of based on real-time, intraoperative imaging, the target location may not precisely correspond to the actual lesion location while the patient is on the table, leading to a source of error known as CT-to-body divergence. Also, because it is a virtual representation of both the anatomy and the target based on the preoperative CTs, the fidelity of the virtual bronchoscopy is reliant on the quality of the CT images from which it is derived.
Electromagnetic Navigation Bronchoscopy
Electromagnetic navigation bronchoscopy (ENB) combines virtual bronchoscopy with an electromagnetic field that can precisely track the position of the bronchoscope during the procedure. CT images are used to create a rendering of the airways and airway routes to the target.
Before the procedure begins, an electromagnetic field generator is placed in the proximity of the patient. The guidecatheter with a sensor is placed in the working channel of the bronchoscope so that, as the bronchoscope and catheter is advanced through the airways, the system knows its position and can show on the virtual bronchoscopy the relative location of the catheter to the target, similar to GPS. Once at the target, the clinician can then systematically sample the target area in order to obtain biopsy samples using standard biopsy instruments.
Similar to virtual bronchoscopy alone, the reliance on a preoperative CT for establishing the navigation target means the ENB is also susceptible to CT-to-body divergence and can have its navigational accuracy impacted by this.
The GPS in your car analogy is apropos here as, in your car, the GPS can unerringly guide you to your desired location. The same is true of ENB; ENB can reliably guide the bronchoscopist to the point in space defined as the target but, because the lung is a dynamic environment, that location might not be precisely where the pulmonary lesion is at that point in time during the procedure. Moreover, because there is no intraoperative imaging, it is not possible to confirm tool-in-lesion prior to biopsy, which is why a systematic sampling approach of a wide area, sometimes called “cloud biopsy,” is needed in order to account for this potential error and maximize likelihood that some of the samples will come from the actual lesion. Due to its magnetic nature, ENB also poses the issue of interference with other equipment in the room and patients with pacemakers and other such implants are contraindicated for its use.
Robotic Bronchoscopy
Rather than manually manipulating the bronchoscope, the advent of robotic bronchoscopy platforms like the Ethicon Monarch or Ion by Intuitive, allows physicians to move a mechanized flexible bronchoscope with a controller.

The bronchoscope used in robotic bronchoscopy is typically smaller than those used in traditional bronchoscopy, allowing, in theory, physicians to reach parts of the peripheral lung that may have been challenging to access with traditional bronchoscopy techniques.
As the physician is controlling the robotic system, a 3D virtual bronchoscopy map of the patient’s lung is shown on a computer screen, allowing the physician to follow along and see exactly where the bronchoscope is in relation to the target.
While the added benefits of stability and greater catheter articulation are superior to that of manual catheters used in traditional bronchoscopy, robotic bronchoscopy platforms are
also hindered by the fact that they are still built upon navigation technologies – be they shape-sensing or ENB – that rely on preoperative CT scans to establish the navigation target and so are susceptible to the same CT-to-body divergence errors as the underlying navigation technologies upon which they are based.
Moreover, it has yet to be demonstrated in peer-reviewed literature that robotic bronchoscopy alone without intraoperative imaging, provides an improvement in diagnostic yield compared to ENB and other older navigation technologies used in conjunction with a manual bronchoscope.
There have been studies that have shown diagnostic yields in the 80 and 90 percent range with robotic bronchoscopy, but virtually all such reported outcomes are confounded by the fact that those studies paired robotic bronchoscopy with intraoperative CT imaging such as cone-beam CT (CBCT) which, alone, has been shown to contribute to a higher diagnostic yield.
The high cost of the robotic bronchoscopy platforms both in terms of initial capital outlay as well as ongoing per-procedure operational costs also limits its viability outside of major academic centers and metropolitan hospitals in the United States and will be a barrier to entry in more cost-sensitive markets outside the United States.
Radial Probe Endobronchial Ultrasound (R-EBUS)
The R-EBUS probe technique uses a miniature, rotating ultrasound probe inserted down the working channel of a bronchoscope to provide an ultrasound signal that can provide an indication as to whether or not the probe is in a lesion or not due to the fact that a lesion and healthy parenchyma tissue of the lung have differing echodensities that can be detected using a R-EBUS probe. Because A R-EBUS probe returns a signal versus an actual image and the signal is not directional, the technology is not used for bronchoscopy navigation, but rather as another data point to confirm that the bronchoscope is at the lesion during a procedure.
Besides fluoroscopy, R-EBUS bronchoscopy is the only other bronchoscopy technology that provides real-time information versus a static snapshot of a point in time.
CT-Guided Bronchoscopy
High resolution three-dimensional CT imaging generates real-time images to help navigate bronchoscopy instruments directly to the target lesion for biopsy. Intraoperative CT scans can also provide visual confirmation that tools have successfully penetrated the lesion.
Leveraging intraoperative CT, bronchoscopists are able to achieve diagnostic outcomes similar to that achieved by interventional radiologists with a less invasive approach.
One such technique is cone-beam CT (CBCT), a computational tomographic X-ray imaging modality that allows for accurate, 3D imaging of tissue at a submillimeter resolution.
The advent of 3D-capable C-arms, often referred to as “mobile cone-beam,” has attempted to make CBCT more accessible to bronchoscopists. However, the technology remains newer and some of the concerns of fixed CBCT systems such as high cost and comparatively high radiation exposure, still remain a concern.
Moreover, these new 3D C-arms, while able to render 3D tomographic images, tend to also be of lower resolution than fixed CT systems and so cannot image soft-tissues and particularly smaller, less dense lung lesions, with the same fidelity as full-sized, fixed CBCT systems let alone full-fledged CT scanners.
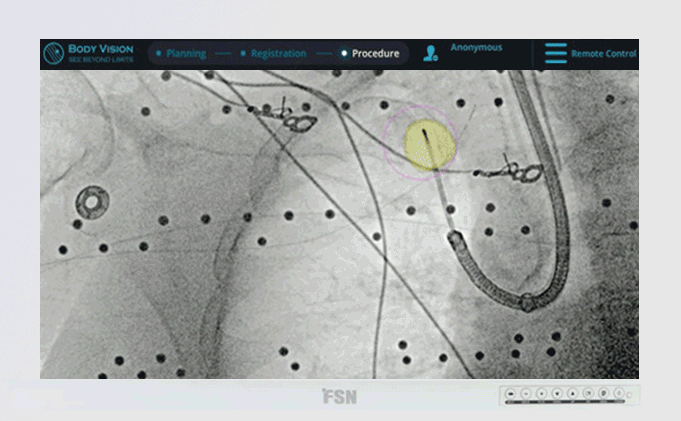
Body Vision Medical’s LungVision™ system uses artificial intelligence (AI) to transform X-ray images from any C-arm into real-time, intraoperative CT scans which can be presented in multiple views that enable bronchoscopists to see both the lesion and their bronchoscopic tools in real-time during the procedure.
Body Vision’s LungVision system also provides navigational capabilities, enabling it to serve as an all-in-one diagnostic bronchoscopy solution that supplants electromagnetic navigation bronchoscopy (ENB) platforms or as a dedicated imaging platform that enhances robotic bronchoscopy platforms by providing real-time, intraoperative CT imaging.
Bronchoscopy Process Phases
Though each bronchoscopy technique has its own particular intricacies in terms of process, the general bronchoscopy procedure can be explained in a few key phases.
- First, a sedative is given to the patient to help them relax for the procedure
- An anesthetic is applied to the throat, mouth, or nose depending on the particular procedure
- Next, the bronchoscope is inserted into the patient
- A saline solution is sent through the working channel of the bronchoscope to collect samples in a process called “lavage”
- R-EBUS bronchoscopy, CT imaging, electromagnetic navigation, or other bronchoscopy techniques may be used to assist in guiding instruments to the intended biopsy site
- Biopsy needles, forceps, cryoprobes, or other instruments may be passed through the working channel of the bronchoscope for biopsy
- Finally, the bronchoscope is removed
Selection of a Biopsy Modality
Not all patients with peripheral lung lesions need to be biopsied. For those with small or stable lesions, CT surveillance is usually sufficient. However, a surgical biopsy may be preferable for patients whose lesions are at a high risk of malignancy. Patients with an intermediate risk of malignancy can benefit from non-surgical biopsy techniques, like image-guided bronchoscopy.
Once pulmonary peripheral lesions have been confirmed for biopsy, a specific biopsy modality must be selected. Patients with lesions requiring nonsurgical biopsy have the greatest range of biopsy options. The particular type of biopsy can be determined by:
- Size of the lesion
- Lesion location
- Suspected diagnosis
Typical options include a transthoracic biopsy needle, diagnostic bronchoscopy, or surgical resection. But there are also cutting-edge biopsy modalities to consider.
Body Vision’s image-guided approach leverages the power of artificial intelligence to enable the use of a C-arm to generate intraoperative CT scans for accurate navigation to the lesion. LungVision™ also eliminates the need to take random biopsy samples, as the addition of intraoperative CT imaging enables visualization of the actual lesion and lesion location during the procedure, enabling physicians to precisely acquire tissue from within the lesion, maximizing likelihood for a definitive diagnosis.
There’s no one most advantageous biopsy technique, but there are a few common practices agreed upon by most experts.
- CT-guided transthoracic needle biopsy is usually preferable for lesions close to the periphery of the chest wall or deep within the respiratory system. Transthoracic needle aspiration generally garners a higher diagnostic yield than an image-guided system.
- Diagnostic bronchoscopy with or without adjunctive technologies such as robotic bronchoscopy, electromagnetic-guided bronchoscopy, radial probe endobronchial ultrasonography, and/or intraoperative CT-guidance is typically accepted as appropriate alternatives to CT-guided transthoracic needle biopsy and have demonstrated to have fewer complications, though, at least historically without the assistance of intraoperative CT guidance, at the expense of diagnostic success.
- If image-guided or transthoracic needle techniques fail to yield a sufficient diagnosis, a surgical biopsy may be necessary.
It should be noted that not every medical facility has the resources or staff to reasonably perform these bronchoscopic biopsy techniques, and conventional bronchoscopy may be the only option available.
Potential Complications
Image-guided bronchoscopy for peripheral lung lesions can be highly successful, resulting in definitive diagnosis and higher diagnostic yields. However, like any medical procedure, image-guided bronchoscopy also comes with its potential complications.
Overall, complication rates are typically low for this procedure. Image-guided bronchoscopy is well-tolerated by patients and complications have been recorded to be as low as 0-8%.
Image-guided bronchoscopy techniques use standard operating instruments such as forceps and needles and are performed in combination with sedation. Much like a conventional bronchoscopy, any potential complications from the procedure are mostly due to procedural or sedative factors such as bleeding or hypotension.
One of the most common complications of a bronchoscopy is pneumothorax or a collapsed lung. However, even this is relatively rare during bronchoscopy, occuring in fewer than five percent of cases, and is much more likely to occur as a result of a biopsy procedure involving a transthoracic needle.
More common still is bleeding as the result of a bronchoscopy. Blood loss is typically negligible, between 100 to 300 mL, and does not require additional procedures to treat.
The Body Vision Advantage
Body Vision offers physicians AI-driven, intraoperative CT imaging during diagnostic bronchoscopy that is clinically proven to maximize diagnostic yield. We understand the threat that lung cancer poses to public health and have made it our mission to save lives through the democratization of innovative medical technologies.
Body Vision's C-Arm Based Tomography showing tool-in-lesion confirmation.
Our LungVision™ System is compatible with existing imaging and bronchoscopy equipment in order to help healthcare institutions provide optimal care without increasing overall operating costs. Our technology enables institutions to drive superior clinical outcomes with reduced radiation and greater accessibility compared to CBCT.
Body Vision’s AI-driven intraoperative imaging platform maximizes the likelihood of obtaining a definitive diagnosis for lung patients. Higher diagnostic success results in greater patient retention. Accordingly, our cutting-edge image-guided bronchoscopy technology can elevate the visibility of the lung program and serve as a point of differentiation for an institution, driving growth in market share.
The LungVision™ System provides a comprehensive, cost-effective image-guided bronchoscopy solution. The cost-effectiveness of the LungVision™ System is especially attractive for regional and community hospitals, reducing the need for patients to travel great distances in order to access care.
The LungVision™ System is powered by cutting-edge artificial intelligence. We’ve engineered the main unit to be as discreet and mobile as possible so it can neatly fit into even the most confined spaces.
A wireless tablet is used to control the LungVision™ System, giving doctors the flexibility to move around freely while managing the procedure. For those looking to use Body Vision as a complete, end-to-end navigation bronchoscopy solution, we offer a disposable procedural kit, compatible with most bronchoscopes.
At Body Vision, we’re committed to democratizing access to high-quality advanced image-guided bronchoscopy technology in operating rooms across the world. We know the value of treating peripheral pulmonary lesions early for the continued health and well-being of patients.
With nearly 2,000 patients who have already benefited from its AI-driven, intraoperative imaging technology, Body Vision is committed to partnering with institutions, physicians and staff worldwide to improve lung cancer diagnosis so that lung cancer patients globally can have hope for longer, healthier lives.
FAQs
What is guided bronchoscopy?
A guided bronchoscope leverages navigational technology to direct medical instruments to a target for diagnostic or therapeutic purposes such as biopsy or surgical resection.
What are the risks when undergoing a bronchoscopy??
Bronchoscopy procedures generally yield few complications and may only result in soreness or mild pain around the throat and mouth following the procedure. Bronchoscopy is typically an outpatient procedure with no required hospital stay for patients.
How does bronchoscopy help diagnose lung cancer?
Bronchoscopy is useful in collecting biopsies from pulmonary lesions and lymph nodes from which pathology labs can then use to diagnose whether the lesion is malignant or benign and, if malignant, provide lung cancer staging.