Lesion Characteristics
Lesion Size (diameter): 11mm
Lesion Location: Right Upper Lobe (RUL)
Visible on Fluoro: No
Case Information
Full Procedure Time: 65 Minutes
Final Pathology Report: Granulomatous inflammation with necrosis
Patient Background
A former remote smoker female presented with a lesion in the right upper lobe (RUL) on CT. To determine the best treatment a diagnostic bronchoscopy was scheduled to obtain tissue samples from the lesion.
The Procedure
Planning
During the planning of the LungVision™ system, a preoperative CT scan is uploaded and the lesion is identified and outlined to provide the system with an estimate of its size, shape, and location before the procedure begins. The LungVision system leverages the airway data extracted from the preoperative CT scan to generate a virtual bronchoscopy (VB). This visualization technique creates a virtual representation of the bronchial pathways and highlights the optimal route to reach the lesion. LungVision was used as a standalone system for both navigation and real-time intraoperative imaging to enable navigation, tool-in-lesion confirmation, and biopsy from this 11mm lesion in the right upper lobe.
Registration
Once the patient is positioned on the table, the LungVision registration process involves two rotations of the C-arm. The first spin is centered around the main carina, while the second spin is around the lesion itself. These C-arm spins generate an initial C-Arm Based Computed Tomography (CABT) scan which serves to confirm the precise location of the lesion prior to navigation. In this particular case, LungVision was used in conjunction with a Siemens Cios Spin C-arm operating in standard 2D mode. This combination allowed for the creation of real-time, intraoperative 3D scans with approximately 1/6th of the radiation that would typically be emitted during a Cios Spin 3D spin.

Marking the main carina on LungVision’s CABT during registration.
 Lesion marking on LungVision’s C-Arm Based Tomography during registration.
Lesion marking on LungVision’s C-Arm Based Tomography during registration.
Navigation
Navigation to the lesion was completed under the guidance of LungVision’s virtual bronchoscopy and real-time augmented fluoroscopy. A LungVision™ procedural kit served as a pre-curved extended working channel to better access the lesion. Its radiopaque markers made it easier to see the catheter under fluoroscopy during navigation.

LungVision™ augmented fluoroscopy and real-time lesion location during navigation. Note the radiopaque markers of the LungVision catheter which make it easier to see under fluoroscopy.
Tool-in-Lesion Confirmation
Once in close proximity to the lesion, as shown on LungVision’s real-time augmented fluoroscopy, another C-arm spin is performed to visually confirm tool-in-lesion in multiple 3D planes. Because this imaging is captured in real-time, CT-to-body divergence is eliminated. This spin confirmed that the tool was in the lesion.

LungVision™ C-Arm Based Tomography (CABT) imaging showing tool-in-lesion confirmation.

LungVision™ AI Tomography imaging showing tool-in-lesion confirmation.

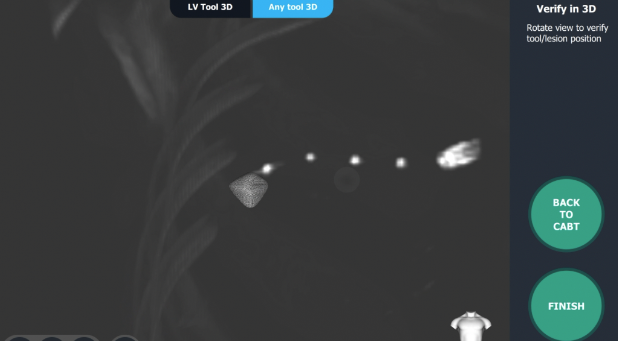
LungVision™ interactive 3D View of the intraoperative CT scan providing tool-in-lesion confirmation.
Biopsy
LungVision’s augmented fluoroscopy provided the real-time imaging necessary to confirm tissue samples were acquired from within the lesion during biopsy. A pair of biopsy forceps were used to acquire samples.

Biopsy via forceps under LungVision’s real-time augmented fluoroscopy.
Final Pathology and Treatment
The final pathology report indicated granulomatous inflammation with necrosis. A three-month follow-up CT showed the nodule was stable.
Conclusion
LungVision™ provided the image-guided navigation and real-time intraoperative CT imaging during navigation and biopsy that enabled the precise navigation to this 11mm RUL lesion, visual tool-in-lesion confirmation, and the image-guided biopsy approach that resulted in a definitive negative cancer diagnosis on this patient.
About Dr. Sethi
Sonali Sethi, MD
Interventional Pulmonologist
Cleveland, Ohio