

John Muir Health, Concord Medical Center
Concord, CA
Type of Facility: Short Term Acute Care
Type of Control: Voluntary Non-profit
Total Staffed Beds: 244
Total Patient Revenue: $3,921,023,108
Total Discharges: 11,522
Total Patient Days: 58,403
LungVision® Acquisition: 2023

Wilson Tsai, MD
Prometheus Medical Innovations.
Director of the Thoracic Surgical Program, John Muir Health
LungVision® Trained: 2023
Background
Dr. Wilson Tsai had built a leading robotic-assisted thoracic surgery (RAS) program and was performing both a bulk of the navigational bronchoscopies to diagnose lung cancer as well as performing robotic lung resection on patients that either were definitively diagnosed with lung cancer or had a suspicious pulmonary nodule that had a high probability of cancer.
Dr. Tsai was seeking a real-time imaging solution that:
- Augmented the capabilities of the Auris Monarch and later the Ion by Intuitive robotic bronchoscope to overcome CT-to-body divergence and maximize the likelihood of a definitive diagnosis, particularly on smaller lesions that might be early-stage cancer
- Had a shallow learning curve so that the interventional pulmonology team at John Muir Health could take on more of the navigational bronchoscopy cases, enabling Dr. Tsai to focus on surgical resection
- Seamlessly integrates into a technology-rich OR to streamline Dr. Tsai’s innovative SABRE (Single Anesthetic Bronchoscopic Robotic Event) protocol which involved robotic-assisted bronchoscopy (RAB) followed by a robotic lung resection in a single anesthesia event.
Acquired LungVision® in June, 2023.
Clinical and Financial Impact
Data provided by Wilson Tsai, MD
Takeaway
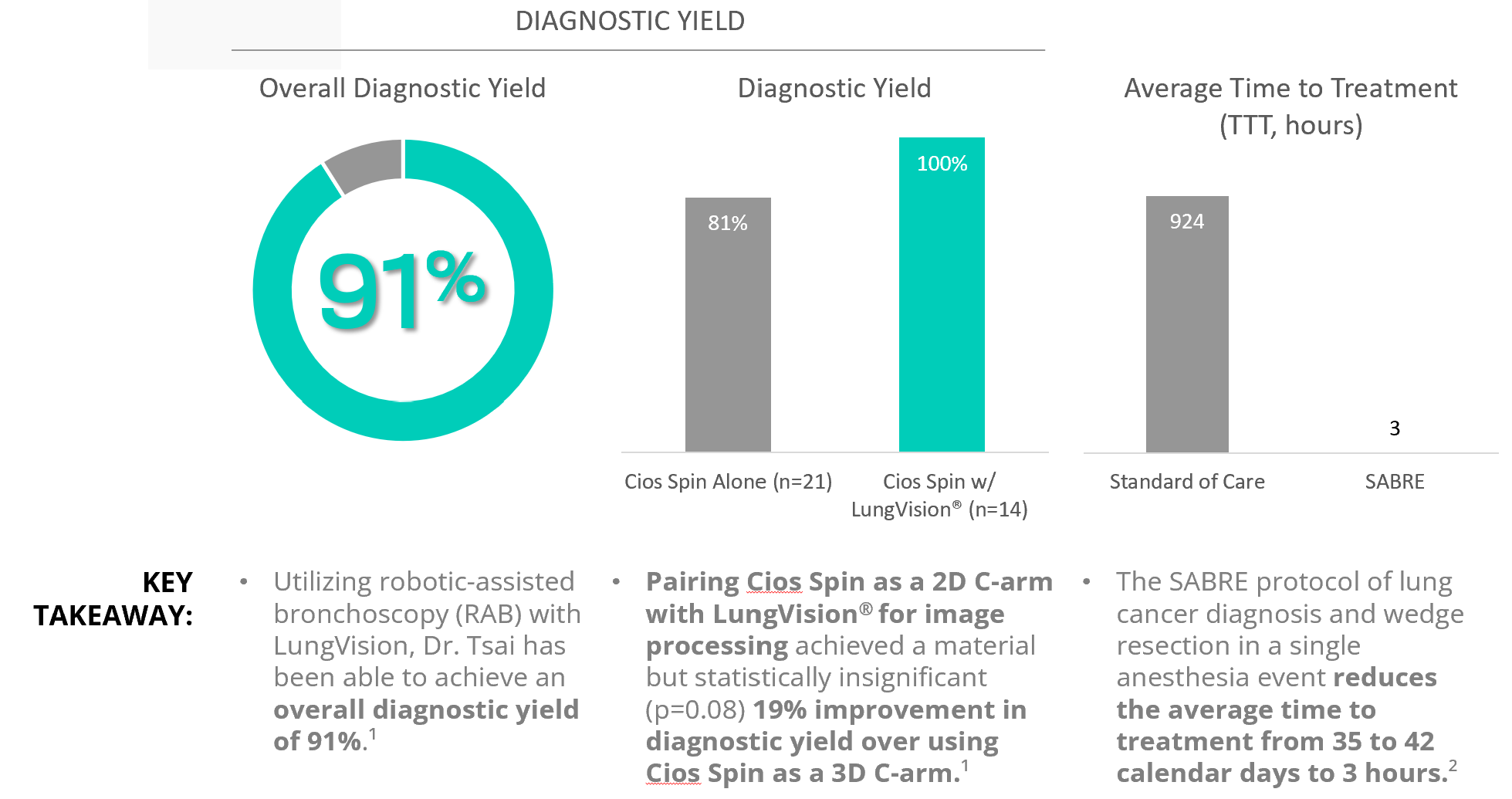
Utilizing LungVision® AI-driven real-time imaging paired with robotic bronchoscopy for more precise endobronchial lung nodule biopsy and ICG-soaked fiducial coil placement for subsequent wedge resection in cases of lung cancer diagnosis, Dr. Tsai was able to drive a 91% overall diagnostic yield.¹
Empowered by LungVision® real-time imaging to maximize likelihood of a definitive diagnosis via endobronchial lung nodule biopsy, the SABRE single-anesthesia event protocol enabled the thoracic surgery program to reduce average time to treatment (TTT) from 35 to 42 calendar days to 3 hours.²
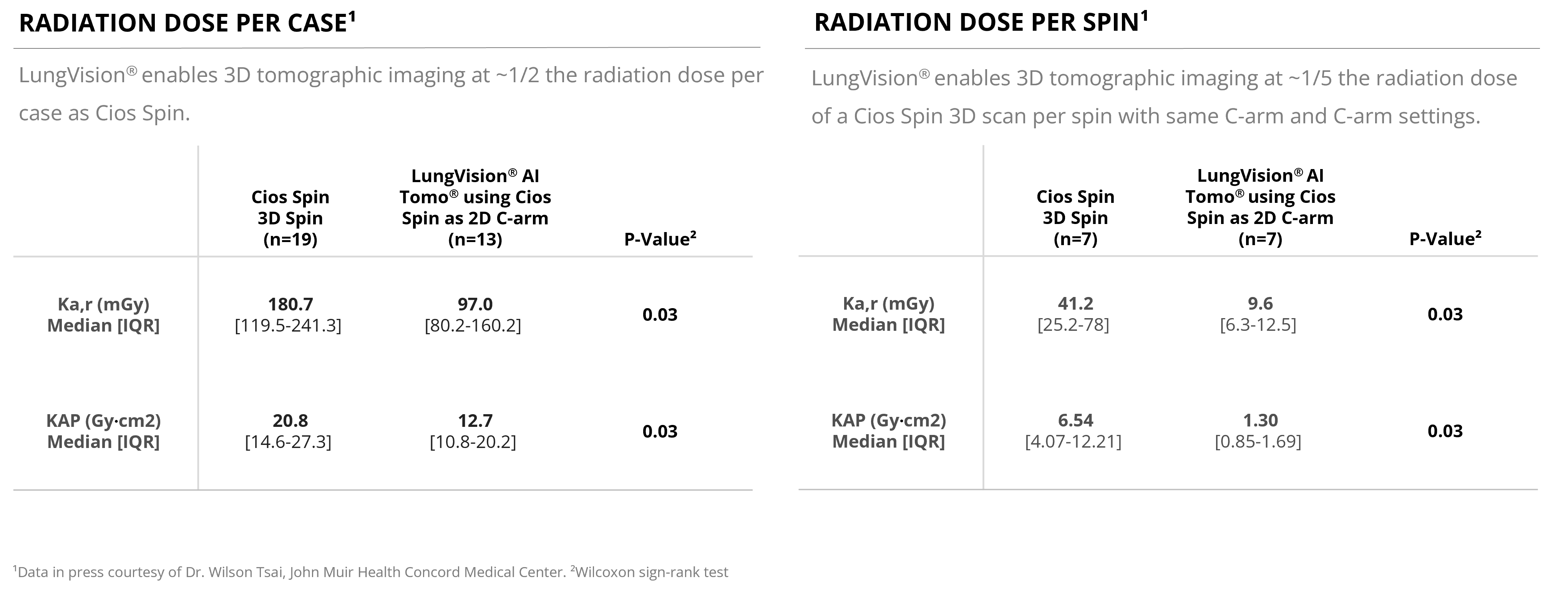
Compared with using a Cios Spin as a 3D C-arm, the combination of Cios Spin as a 2D C-arm with LungVision’s proprietary AI-driven tomographic imaging algorithm was able to produce same if not better quality intraoperative tomographic imaging at < 1/5 the radiation spin-for-spin.¹