The State of Lung Cancer Today
Today, lung cancer ranks as the second most prevalent cancer globally, with approximately 2.2 million new cases annually. Its low five-year survival rate, below 20%, positions it as the leading cause of cancer-related deaths worldwide, resulting in 1.8 million annual fatalities. The primary reason behind this bleak survival rate is that only 16% of lung cancer patients receive an early-stage diagnosis, offering a more hopeful five-year survival rate of 56%. Tragically, the majority of lung cancer cases are diagnosed at advanced stages, where survivability drops to a mere 5%, and over half of those diagnosed succumb within a year.¹
The Issue with Semi-Solid Nodules
Obtaining sufficient tissue from suspicious lung lesions for a definitive diagnosis has long been difficult in diagnostic bronchoscopy because of bronchoscopist’s inability to visualize lesions in real-time and visually confirm tool-in-lesion during lung nodule biopsy. This is all the more challenging with semi-solid and non-solid lesions like ground glass opacities (GGOs) because their inherent lack of density makes them impossible to see with traditional 2D fluoroscopy and potentially difficult to visualize even on tomographic scans.
Semi-solid nodules are detected in approximately 9% of patients undergoing routine CT lung cancer screening. Despite their comparatively slower growth and metastasis, early identification of these semi-solid nodules remains crucial as they carry a higher malignancy risk compared to their solid lesion counterparts and the incidence of cancer in GGOs has been reported as high as 63%.2,3,4 Thus, real-time imaging that enables visualization of semi-solid lesions such as GGOs is all the more important during lung nodule biopsy to maximize the likelihood of achieving tissue adequacy and obtaining a definitive diagnosis.
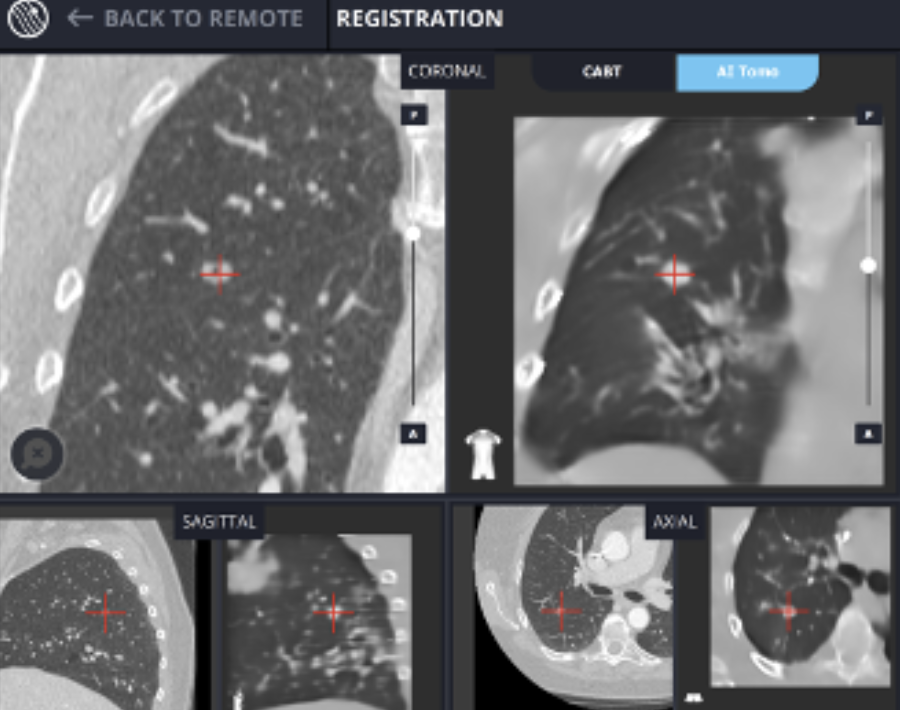
LungVisionTM is the only advanced navigation system that does not rely on a preoperative CT but rather relies on the data acquired from a conventional C-arm spin to update lesion location in real-time during the procedure. Moreover, LungVision’s AI Tomography imaging technology enables bronchoscopists to visualize even GGOs intraoperatively, allowing them to confidently obtain biopsies from these semi-solid and non-solid pulmonary lesions nodules.
GGO Lesion Imaging Library
8.5mm RUL semi-solid, cavitary nodule
LUL GGO
LUL semi-solid lesion of -700 Hounsfield units (HU)
The LungVisionTM Solution: Aiding the Visualization of Semi-Solid Lesions
The LungVisionTM technology leverages artificial intelligence (AI) to convert X-ray images from any C-arm into real-time intraoperative CT scans. This technology empowers bronchoscopists to observe the lesion and its precise location during diagnostic bronchoscopy, providing image-guided navigation and visual confirmation of tool-in-lesion prior to and during biopsy. This innovative approach increases the likelihood of diagnosing lung cancer at an earlier stage when treatment options are more abundant, and survival rates are higher.
Sources
1. Association, A. L. (n.d.). Lung cancer fact sheet. American Lung Association. https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancer-fact-sheet#:~:text=The%20lung%20cancer%20five%2Dyear,and%20prostate%20(98.2%20percent).&text=The%20five%2Dyear%20survival%20rate,localized%20(within%20the%20lungs
2. Pulmonary ground-glass opacity (GGO) lesions–large ... - sciencedirect. (n.d.). https://www.sciencedirect.com/science/article/pii/S1556086415321079
3. Migliore, M., Fornito, M., Palazzolo, M., Criscione, A., Gangemi, M., Borrata, F., Vigneri, P., Nardini, M., & Dunning, J. (2018, March). Ground glass opacities management in the lung cancer screening era. Annals of translational medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5890046/
4. Hammer, M. M., & Hatabu, H. (2020, September 4). Subsolid pulmonary nodules: Controversy and perspective. European journal of radiology open. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7481135/